Key Takeaways
- Properly managed psychiatric medications are a critical component of recovery for individuals with co-occurring mental health and substance use disorders.
- Not all psychiatric medications carry addiction risk. Non-addictive options like SSRIs, SNRIs, and mood stabilizers can be safely used throughout recovery.
- Medication changes should never be made without medical supervision, as abrupt discontinuation can trigger withdrawal, relapse, or psychiatric crisis.
- Effective medication management requires ongoing communication between the prescribing psychiatrist, therapists, and the client throughout all phases of recovery.
- Stigma around psychiatric medication in recovery communities is outdated and harmful. Using prescribed medication to treat a diagnosed condition is not the same as substance abuse.
The Role of Mental Health Medications in Recovery
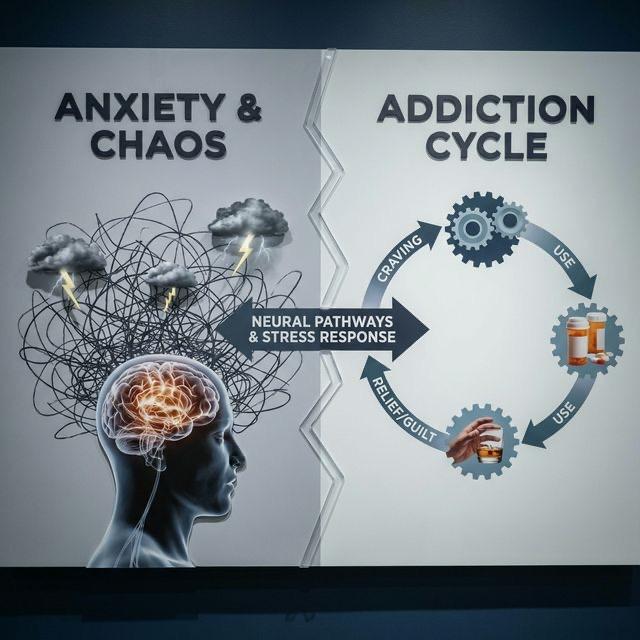
Managing mental health medications during recovery is one of the most important and misunderstood aspects of dual diagnosis treatment. For individuals with co-occurring mental health and substance use disorders, psychiatric medications often play a vital role in stabilizing mood, reducing anxiety, managing psychotic symptoms, and creating the emotional foundation necessary for meaningful therapeutic work.
Yet many individuals in recovery receive conflicting messages about medication. Some recovery communities emphasize total abstinence from all mood-altering substances, inadvertently discouraging the use of prescribed psychiatric medications. Others lack the medical expertise to differentiate between medications that carry addiction risk and those that do not. These misconceptions can lead people to abandon medications they genuinely need, with potentially devastating consequences.
At Trust SoCal in Southern California, our medical team provides expert psychiatric medication management that is fully integrated with our addiction treatment program. We believe that informed, evidence-based medication use is a tool for recovery, not an obstacle to it.
Understanding Medication Categories
Not all psychiatric medications are created equal when it comes to addiction risk. Understanding the different categories of medications helps individuals in recovery make informed decisions about their treatment in collaboration with their prescribing physician.
Non-Addictive Psychiatric Medications
The majority of psychiatric medications used to treat depression, anxiety, bipolar disorder, and psychotic disorders carry no addiction potential whatsoever. Selective serotonin reuptake inhibitors like sertraline, fluoxetine, and escitalopram work gradually over several weeks and do not produce euphoria, intoxication, or cravings. They are universally considered safe for use in individuals with substance use histories.
Mood stabilizers including lithium, valproate, and lamotrigine are similarly non-addictive. Atypical antipsychotics such as quetiapine, aripiprazole, and olanzapine have no abuse potential. These medications address the underlying neurochemical imbalances that drive psychiatric symptoms without activating the brain's reward circuits in ways associated with addiction.
Medications Requiring Careful Monitoring
A smaller category of psychiatric medications does carry some abuse potential and requires more careful management in individuals with addiction histories. Benzodiazepines such as alprazolam, clonazepam, and lorazepam are effective for anxiety and insomnia but produce sedation, euphoria, and physical dependence that make them problematic for many people in recovery.
Stimulant medications used for ADHD, including methylphenidate and amphetamine-based formulations, also require careful consideration. While they are therapeutically appropriate for some individuals in recovery, their use must be closely monitored. Extended-release formulations with lower abuse potential are generally preferred over immediate-release options.
Medication-Assisted Treatment for Addiction
Medications specifically designed to treat substance use disorders, including buprenorphine, methadone, naltrexone, and acamprosate, represent a distinct category. These medications reduce cravings, block euphoric effects, or manage withdrawal symptoms, directly supporting the addiction recovery process.
Despite ongoing stigma, medication-assisted treatment is strongly supported by research and endorsed by every major medical organization. Using these medications is not substituting one addiction for another. It is treating a medical condition with appropriate pharmacotherapy, no different from using insulin for diabetes or antihypertensives for high blood pressure.
Common Concerns About Medications in Recovery
Individuals in recovery frequently express concerns about psychiatric medications that can prevent them from accessing needed treatment. Addressing these concerns with accurate information is an essential part of comprehensive dual diagnosis care.
Am I Trading One Addiction for Another?
This is perhaps the most common concern, and the answer depends entirely on the medication in question. Taking an SSRI for depression is categorically different from abusing opioids for euphoria. Non-addictive psychiatric medications do not produce the compulsive use, tolerance, withdrawal, and loss of control that define addiction. They restore normal brain function rather than hijacking it.
Even medications with some abuse potential, such as buprenorphine for opioid use disorder, function differently in a therapeutic context than drugs of abuse. They produce stable, even levels of receptor activation rather than the surge-and-crash pattern that drives compulsive use. The distinction between therapeutic medication use and substance abuse is clear and well-established in medical literature.
Taking medication for a psychiatric condition is no more a sign of weakness than taking medication for a heart condition. Both are medical treatments for medical conditions.
— Dr. Nora Volkow, Director of the National Institute on Drug Abuse
What If My Recovery Group Disapproves?
Some twelve-step groups and recovery communities have historically discouraged the use of psychiatric medications, viewing them as incompatible with sobriety. While this attitude has softened considerably in recent years, it persists in some circles and can pressure individuals to discontinue needed medications.
All major twelve-step organizations, including Alcoholics Anonymous, have official positions supporting the appropriate use of prescribed psychiatric medications. If you encounter disapproval in a specific group, seek a different meeting or group that is medication-friendly. Your medical treatment decisions should be made with your doctor, not your peer group.
Medication Management During Different Phases of Recovery
Mental health medications during recovery require different management strategies depending on the phase of treatment. What is appropriate during acute detox differs from what is needed during residential treatment, outpatient care, or long-term maintenance.
During Detox and Early Recovery
The detox phase presents unique medication challenges because withdrawal symptoms can mimic or mask psychiatric conditions. Medications used during detox, such as benzodiazepines for alcohol withdrawal or clonidine for opioid withdrawal, are typically short-term and should not be confused with ongoing psychiatric treatment.
Starting or adjusting long-term psychiatric medications during active detox requires particular care. Our medical team at Trust SoCal evaluates each client's pre-existing medication regimen, maintains medications that are clearly needed, and delays new prescribing decisions until the acute withdrawal phase has passed and a clearer diagnostic picture emerges.
During Active Treatment
The residential or intensive outpatient phase of treatment provides an ideal opportunity for careful medication optimization. Clients are in a controlled, supportive environment where medication effects and side effects can be closely monitored. Dosage adjustments can be made with daily observation and rapid clinical response.
This phase is also when the distinction between substance-induced and independent psychiatric conditions becomes clearer. Symptoms that persist after several weeks of sobriety are more likely to represent independent conditions warranting ongoing medication. This information guides long-term medication planning.
During Long-Term Recovery
Medication management during long-term recovery requires a plan for ongoing psychiatric follow-up. Relying solely on a primary care physician for complex psychiatric medication management is often inadequate. Regular appointments with a psychiatrist who understands addiction ensure that medications remain appropriate and that emerging symptoms are addressed promptly.
Medication needs may change over time as recovery progresses. Some individuals can eventually taper off psychiatric medications under medical supervision as therapy and lifestyle changes provide sufficient symptom management. Others will benefit from indefinite medication use. Both paths are valid and should be determined by clinical outcomes rather than ideology.
The Dangers of Stopping Medications Without Guidance
One of the most serious risks in dual diagnosis recovery is the unilateral decision to discontinue psychiatric medications. This may happen because the individual feels better and assumes they no longer need medication, because they encounter stigma in their recovery community, because of bothersome side effects, or because they associate all medications with their addiction.
Abruptly stopping psychiatric medications can produce dangerous withdrawal syndromes, including SSRI discontinuation syndrome, rebound psychosis, manic episodes triggered by lithium discontinuation, or severe anxiety and seizures from benzodiazepine withdrawal. These withdrawal effects frequently trigger substance relapse as the individual desperately seeks relief from acute distress.
At Trust SoCal, we educate every client about the importance of maintaining prescribed medications and the risks of abrupt discontinuation. When medication changes are warranted, they are made gradually under medical supervision with close monitoring for emerging symptoms.
Never stop taking a psychiatric medication without consulting your prescribing physician. Even medications that are being discontinued should be tapered gradually under medical supervision to prevent withdrawal symptoms and psychiatric destabilization.
Communication Between Providers
Effective medication management in recovery depends on clear, consistent communication between all members of the treatment team. The prescribing psychiatrist must be informed about the client's substance use history, current recovery status, and any cravings or relapse episodes. Therapists must be aware of medication changes that might affect emotional processing or therapy engagement.
At Trust SoCal, this communication happens naturally within our integrated treatment model. Our psychiatrist, therapists, and addiction counselors share a unified medical record and participate in regular treatment team meetings. When clients transition to outpatient care, we ensure that their external providers receive comprehensive records and direct communication about medication plans.
Clients themselves play an essential role in this communication. Being honest with all providers about medication adherence, side effects, cravings, and any impulses to adjust medications independently ensures that the treatment team can respond appropriately and maintain safety.
Medication Management Support at Trust SoCal
Trust SoCal provides comprehensive psychiatric medication management as an integrated component of our dual diagnosis treatment program in Fountain Valley, Orange County. Our board-certified psychiatrist has extensive experience managing medications for individuals with co-occurring mental health and substance use disorders.
We understand that navigating medication decisions during recovery can feel overwhelming. Our medical team is committed to partnering with each client to find the right medication regimen, addressing concerns openly, and providing the education needed for informed decision-making. Contact our admissions team to learn more about our integrated approach to medication management and addiction treatment.

Rachel Handa, Clinical Director
Clinical Director & Therapist