Key Takeaways
- Gabapentin misuse has increased dramatically, with the drug often used to enhance the effects of opioids, alcohol, or other substances, or taken in high doses for its own euphoric and sedative effects.
- Physical dependence on gabapentin develops with regular use, and withdrawal can produce anxiety, insomnia, seizures, and other symptoms requiring medical management.
- Several states have reclassified gabapentin as a controlled substance due to rising abuse rates, though it remains unscheduled at the federal level.
- Individuals with a history of substance use disorders are at significantly higher risk for gabapentin misuse and should be monitored closely if prescribed the medication.
- Treatment for gabapentin dependence involves a medically supervised taper and comprehensive addiction treatment addressing any co-occurring substance use.
The Rise of Gabapentin Misuse
Gabapentin (brand name Neurontin) is a medication originally developed to treat epilepsy and subsequently approved for neuropathic pain. It has also been widely prescribed off-label for anxiety, insomnia, restless leg syndrome, and as an adjunct in addiction treatment. Gabapentin became one of the most commonly prescribed medications in the United States, with over 69 million prescriptions dispensed annually, in part because it was considered to have minimal abuse potential compared to opioids and benzodiazepines.
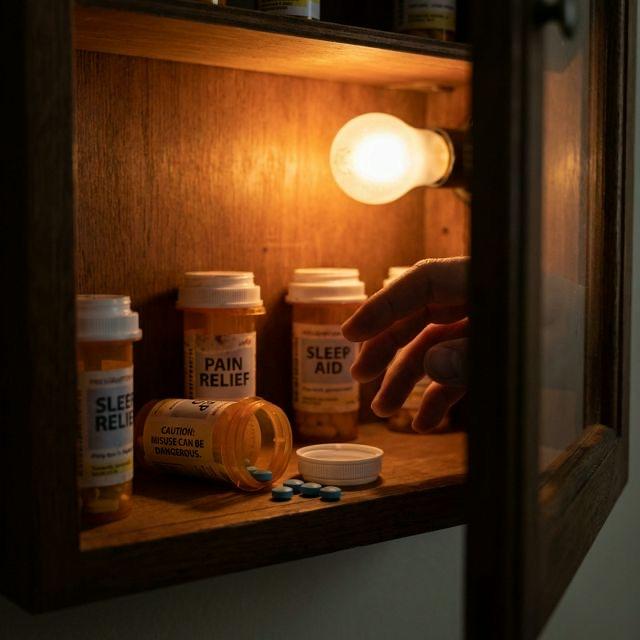
However, this assessment has proven dangerously optimistic. Studies now indicate that 15 to 22 percent of individuals with opioid use disorders misuse gabapentin, and the drug has been increasingly identified in overdose toxicology reports, particularly in combination with opioids. When taken at high doses or combined with other CNS depressants, gabapentin produces euphoria, sedation, and dissociative effects that drive compulsive use in vulnerable populations.
In Orange County and throughout Southern California, gabapentin misuse has become a growing concern in addiction treatment settings. Trust SoCal's clinical team has observed patients presenting with gabapentin as a primary substance of abuse, as well as individuals who use gabapentin alongside opioids to enhance euphoric effects or potentiate the opioid high. Addressing this trend requires awareness among both prescribers and treatment providers.
As of 2024, several states including Kentucky, West Virginia, Tennessee, Alabama, Michigan, and Virginia have classified gabapentin as a Schedule V controlled substance. California does not currently schedule gabapentin but requires electronic prescription monitoring.
How Gabapentin Is Misused
Gabapentin misuse takes several forms, each carrying distinct risks. The most common pattern involves taking the medication at doses far exceeding the prescribed amount, sometimes consuming 3,000 to 5,000 mg or more in a single session when the typical therapeutic dose ranges from 300 to 1,800 mg daily. At these supratherapeutic doses, gabapentin produces effects described as euphoria, relaxation, and a dissociative or floating sensation.
A particularly dangerous pattern involves combining gabapentin with opioids. Gabapentin enhances and modifies the opioid high, producing effects that users describe as more intensely pleasurable than either substance alone. This combination significantly increases the risk of fatal respiratory depression, as both substances independently suppress breathing and their combined effect is potentiated. Gabapentin has been identified as a contributing factor in an increasing percentage of opioid overdose deaths.
Other misuse patterns include using gabapentin to potentiate alcohol effects, using it as a substitute when preferred substances are unavailable, and combining it with benzodiazepines for enhanced sedation. Individuals in addiction recovery may also misuse gabapentin prescribed for anxiety or pain, particularly if their treatment provider is unaware of the medication's abuse potential in this population.
- Taking doses far exceeding prescribed amounts for euphoric effects
- Combining with opioids to enhance the opioid high
- Using with alcohol to amplify sedation and intoxication
- Obtaining gabapentin from multiple prescribers or purchasing it illicitly
- Using as a substitute when primary drugs of abuse are unavailable
- Combining with benzodiazepines for compounded CNS depression
- Staggering doses throughout the day to maintain effects continuously
Gabapentin Withdrawal Symptoms
Physical dependence on gabapentin develops with regular use, even at prescribed doses, and can produce a withdrawal syndrome that ranges from uncomfortable to medically serious. Gabapentin withdrawal symptoms typically begin 12 to 48 hours after the last dose and may persist for 7 to 10 days, with some symptoms lingering for weeks in individuals who used high doses for extended periods.
The most concerning withdrawal complication is seizures. Because gabapentin modulates neuronal excitability, abrupt cessation can produce rebound excitation similar to the mechanism underlying alcohol and benzodiazepine withdrawal seizures. While the seizure risk with gabapentin withdrawal is lower than with benzodiazepines, it is real enough to warrant medical supervision during discontinuation, particularly in individuals using high doses.
Other withdrawal symptoms include anxiety, insomnia, nausea, sweating, pain sensitivity, agitation, and confusion. Some individuals experience a pronounced rebound effect of whatever symptoms the gabapentin was originally prescribed to treat, such as worsened pain or anxiety that temporarily exceeds pre-treatment levels. This rebound effect can be distressing and may drive relapse if not managed with appropriate clinical support.
Never stop gabapentin abruptly without medical guidance, even if you have been taking it as prescribed. The seizure risk associated with sudden cessation requires a gradual, medically supervised taper.
The Gabapentin-Opioid Connection
The relationship between gabapentin and opioid misuse deserves particular attention because of its prevalence and lethality. Studies have found that gabapentin is present in 8 to 15 percent of opioid overdose deaths, and this percentage has been increasing. The combination is dangerous because gabapentin potentiates opioid-induced respiratory depression through mechanisms that are distinct from but complementary to the opioid's direct effect on brainstem respiratory centers.
Some individuals are prescribed gabapentin by physicians who are aware of their opioid use disorder, intending the medication to help manage pain or anxiety without resorting to additional opioid prescriptions. While this clinical reasoning is understandable, it can inadvertently provide a substance-prone individual with a medication that enhances the very opioid effects they are struggling to overcome. Close monitoring and transparent communication between patient and prescriber are essential.
In addiction treatment settings, gabapentin is sometimes used therapeutically to manage anxiety, insomnia, or alcohol withdrawal. When used in this context for patients with histories of substance misuse, careful risk-benefit assessment and close monitoring are warranted. Trust SoCal's medical team evaluates each patient's complete substance use history before considering gabapentin as part of any treatment protocol.
Treatment for Gabapentin Dependence
Treatment for gabapentin dependence begins with a medically supervised taper, gradually reducing the dose over a period of one to several weeks depending on the dose level, duration of use, and individual response. The taper schedule is individualized, with typical dose reductions of 10 to 25 percent every few days, and careful monitoring for withdrawal symptoms including seizure precautions.
Following stabilization and taper completion, ongoing addiction treatment addresses the behavioral patterns and underlying conditions that drove gabapentin misuse. For individuals who misused gabapentin alongside opioids, treatment must address both substances and their interconnected use patterns. Cognitive behavioral therapy, motivational interviewing, and relapse prevention planning form the therapeutic foundation.
At Trust SoCal in Fountain Valley, our treatment programs are equipped to address gabapentin dependence whether it occurs in isolation or, more commonly, as part of a polysubstance use pattern. Our medical team provides safe detox management, and our clinical team delivers comprehensive therapy that addresses all dimensions of the addiction. Call (949) 280-8360 for a confidential assessment.
If you are prescribed gabapentin and have a history of substance use disorder, discuss the risks openly with your prescriber. Non-addictive alternatives may be available for your condition, and informed prescribing decisions can prevent the development of a new dependency.

Courtney Rolle, CMHC
Clinical Mental Health Counselor